Knowing your baby could stop breathing every time they go to sleep is a terrifying reality that turns your world upside down.
The Sick Children’s Trust runs ten ‘Homes from Home’ across the country, giving families with seriously ill children free accommodation.
The day Sydney-Rose arrived was absolutely terrifying. It was too soon. My baby wasn’t old enough to be born, but I was in a life-threatening condition and too unstable to protest. If doctors didn’t get Sydney-Rose out immediately, then it was likely both of us would die.
Sydney-Rose arrived by emergency caesarean on 6 September 2017 at just 28 weeks. I suffer from renal artery stenosis, which is a narrowing of the arteries that carry blood to the kidneys. This caused my blood pressure to rise to 250/160. 120/80 is considered normal, so this was deadly high. I was also suffering with pre-eclampsia, which was affecting the blood flow through my placenta to my baby. I took myself to A&E at Basildon University Hospital just minutes from where I live. On arrival the doctors had no choice but to deliver Sydney-Rose.
As soon as she arrived, my little baby was taken straight onto the neonatal intensive care unit (NICU). Sydney-Rose was too small, weighing just 1kg, but doctors tried to reassure me that although her lungs were underdeveloped, there were no other complications to her prematurity. For the next three weeks, she remained in an incubator on NICU and I spent all day every day by her side, making the short journey to the hospital every morning and back home every night – trying to get some sleep, though some nights that didn’t happen.
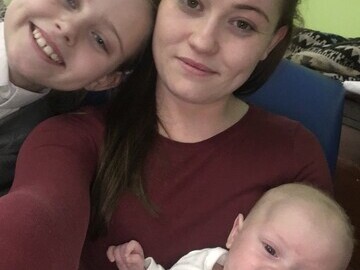
Those three weeks weren’t straightforward. Sydney-Rose didn’t grow stronger as the doctors had anticipated and instead lost 200g and her airway collapsed twice, meaning she had to be intubated. It is so traumatising to see your tiny baby with tubes coming out of her mouth and nose, lying there in an incubator wired up to different machines. I have an older daughter, Kacey-Jo, who was only eight years old at the time, and I was concerned about how distressed being in the hospital was making her feel, but knew I couldn’t keep her away from her baby sister.
At six weeks old, Sydney-Rose became extremely ill with necrotising enterocolitis (NEC). NEC is a serious illness in which tissues in the intestine become inflamed and start to die. Sydney-Rose needed specialist treatment at a different hospital in Cambridge. The Acute Neonatal Transfer Service (ANTS) came to collect us and I travelled alongside my baby in the ambulance to The Rosie Hospital in Cambridge, over 90 minutes from home.
When we arrived at The Rosie Hospital, Sydney-Rose was intubated again and taken to NICU. I watched on helplessly as I rang my sister and asked her to pick up Kacey-Jo from school and drive her to Cambridge to be with us. This is when I heard about Chestnut House. One of the nurses on the ward told me about The Sick Children’s Trust and that there might be a room in a ‘Home from Home’ where we could stay. Kacey-Jo and I stayed in Chestnut House for a week. There was nobody else to look after her, so Chestnut House meant we could be together and there was somewhere away from the hospital environment for us to go, whilst still being only a couple of minutes from Sydney-Rose.
In Chestnut House we could shower and wash, something I had taken for granted before having a seriously ill baby in NICU. I was exhausted – I still hadn’t recovered from the caesarean and was in a lot of pain, plus I needed to have an operation to treat my renal artery stenosis and was suffering as a result. We had got used to eating takeaways whilst Sydney-Rose was in Basildon so it was nice to be able to cook a home-made meal in the kitchen at Chestnut House. The staff were also very supportive and nothing was too much trouble. Kacey-Jo chatted away to them as she watched TV in the living room. Most importantly the ‘Home from Home’ accommodation was free of charge. The financial cost of a hotel would have crippled me.
After a week, Sydney-Rose began making a really good recovery, she was taken off intubation and we were told that she would not need an operation. She was no longer one of the sickest babies on NICU and so we left Chestnut House, as there is such a huge demand on the charity’s ‘Home from Home’ accommodation. For four days we made the three hour round trip to and from The Rosie Hospital until Sydney-Rose was transferred back to our local hospital; it was incredibly draining and the fuel was expensive, but it made us appreciate what a difference Chestnut House had made. Finally, after 11 more days in NICU in Basildon, I brought Sydney-Rose home for the very first time.
Over the next three weeks Kacey-Jo and I got used to having Sydney-Rose at home with us. It felt like the worst was behind us and I could finally start to heal. However, this respite didn’t last long. One day Sydney-Rose just stopped breathing and had to be rushed back into hospital. This time she was transferred by the Children's Acute Transport Service (CATS) to The Royal London Children’s Hospital and admitted onto the paediatric intensive care unit (PICU).
The doctors at The Royal London diagnosed Sydney-Rose with infant apnea of prematurity (AOP). AOP is a condition in which premature infants stop breathing for 15 to 20 seconds during sleep. They told me that AOP is fairly common in preemies, but the doctors also diagnosed her with bronchiolitis caused by an influenza virus, which meant the airways in her already-weakened lungs were infected and inflamed. She needed to be intubated once again and I watched on helplessly, spending a frantic night trying and failing to get some sleep in a small room off PICU.
The Sick Children’s Trust came to my rescue once again and they gave me a room at Stevenson House, another ‘Home from Home’ just minutes from my daughter’s bedside. Irma, the Assistant House Manager, was very welcoming and supportive when I arrived at Stevenson House. I was completely distraught that my daughter was back in hospital – and her kindness meant so much to me at that time.
Although I didn’t spend much time at Stevenson House, as I was by Sydney-Rose’s hospital bedside as much as possible, it was a comfort to have somewhere warm and comfortable to sleep at night. And like Chestnut House, it was also very clean and tidy and also took a bit of the stress away, as I was supporting my baby alone in London and it felt like everyone I knew was a long way away. After one week we were transferred back to our local hospital and the following day allowed home again.
Five weeks later the world was swept from beneath my feet again when Sydney-Rose stopped breathing. It was like déjà vu as she was rushed to another specialist children’s hospital. This time we went to Great Ormond Street Hospital (GOSH).
At GOSH it was worse than before. Sydney-Rose needed intubating for eight days this time and for the first time she was bagged. This meant she manually needed to be ventilated by the nurses with a handheld resuscitation device because without their support, intubation alone was not enough. At the same time, doctors diagnosed her as disabled, suffering from a muscle condition. We won’t know exactly what the diagnosis is until later on in the year, but in the future she will need further tests, continuous physio and child developmental support. So far outside of Basildon Hospital, my baby has had three intensive care stays and been intubated six times. It is reassuring to know that if Sydney-Rose needs further treatment The Sick Children’s Trust will be there for us.
Tate Keating, Sydney-Rose’s mum.
About The Sick Children’s Trust
The Sick Children’s Trust is working to a future where every family with a seriously ill child in hospital will be able to stay together, just minutes from their child’s bed during their treatment.
We believe keeping families together significantly improves the recovery of seriously ill children. We provide free, high-quality ‘Home from Home’ accommodation, as well as emotional and practical support, to families with sick children in hospital in the UK.
The Sick Children’s Trust was founded in 1982 by two paediatric specialists Dr Jon Pritchard and Professor James Malpas. Today we have ten ‘Homes from Home’ at major hospitals around the country where families can stay free of charge, for as long as they need whilst their child is undergoing treatment.
We support around 4,000 families every year, and there is a growing demand for our ‘Homes from Home’ as children must increasingly travel long distances to get the specialist treatment they need. www.sickchildrenstrust.org
Press release distributed by Pressat on behalf of The Sick Children's Trust, on Tuesday 27 February, 2018. For more information subscribe and follow https://pressat.co.uk/
The Rosie Hospital Charity Childcare Home From Home Children Hospital Family Story The Sick Children's Trust Fundraising Charities & non-profits
Published By

020 7638 4066
amy@sickchildrenstrust.org
http://www.sickchildrenstrust.org
Communications Assistant
ryan@sickchildrenstrust.org
Visit Newsroom
You just read:
Knowing your baby could stop breathing every time they go to sleep is a terrifying reality that turns your world upside down.
News from this source: